Pregnancy-related deaths in the U.S. remain a pressing public health crisis, with alarming statistics indicating that over 80 percent of these fatalities are preventable. As the country grapples with the highest maternal mortality rates among high-income nations, recent studies reveal a troubling rise in these numbers from 2018 to 2022. This increase is marked by significant racial disparities in maternal health, where minority groups, especially American Indian and Alaska Native women, experience mortality rates nearly four times higher than their white counterparts. Furthermore, chronic conditions in pregnancy, compounded with inadequate postpartum care, contribute to this disturbing trend. A comprehensive understanding of these maternal mortality rates is essential for developing effective interventions and policies aimed at reducing preventable pregnancy deaths throughout the country.
The alarming surge in fatalities associated with pregnancy in the United States underscores a critical issue in maternal health that demands urgent attention. Often dubbed maternal mortality, this phenomenon highlights the preventable nature of numerous pregnancy-related deaths, which are exacerbated by differences in healthcare access and quality across diverse demographic groups. Additionally, the conditions that lead to these fatalities often stem from inadequate postpartum support and the prevalence of chronic health conditions that can severely complicate pregnancies. Addressing the stark racial disparities in maternal health will be crucial in combating these statistics that reveal how inequities persist in our healthcare systems. Therefore, a multipronged approach focusing on improved healthcare policy, enhanced prenatal and postpartum care, and dedicated resources for at-risk populations is essential to mitigate the increasing rates of mortality related to pregnancy.
Current Trends in U.S. Pregnancy-Related Deaths
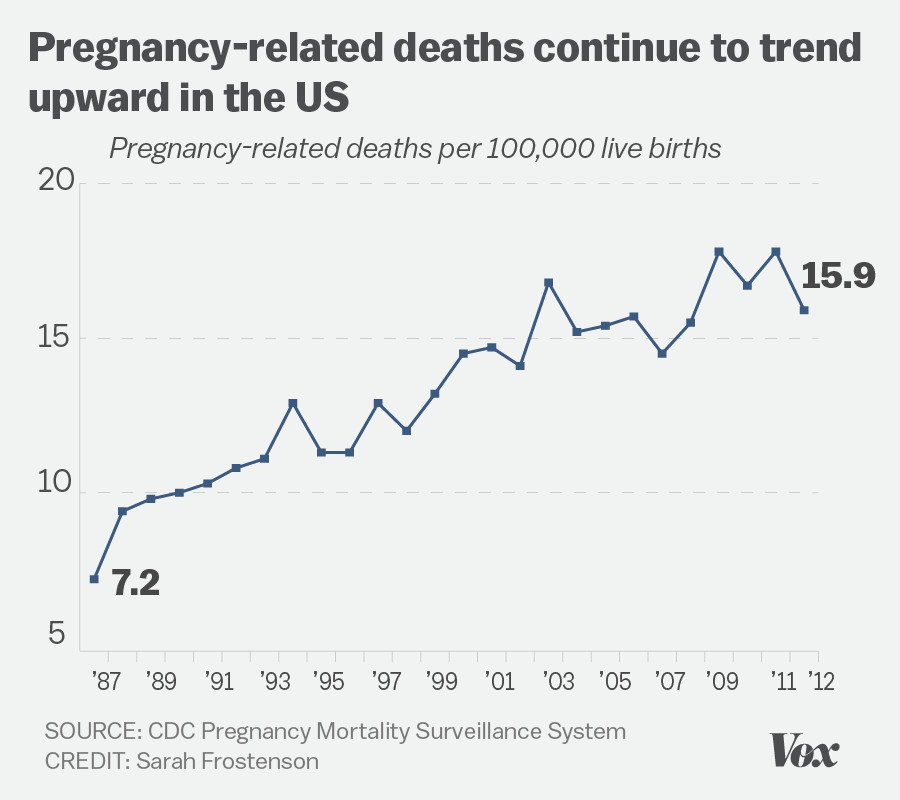
Recent data reveals a troubling rise in pregnancy-related deaths in the U.S., highlighting a critical public health crisis. Between 2018 and 2022, statistics indicated that the maternal mortality rate increased significantly, reaching 32.6 deaths per 100,000 live births by 2022, up from 25.3 in 2018. Alarmingly, over 80% of these deaths are deemed preventable, posing a question about the efficacy and access to prenatal and postpartum care. The findings underscore the urgent need for widespread improvements in maternal healthcare systems to ensure the safety of pregnant individuals across the nation.
Moreover, disparities in maternal health outcomes are stark, with certain racial and ethnic groups facing disproportionately high pregnancy-related death rates. For instance, American Indian and Alaska Native women have mortality rates that are nearly four times higher than their white counterparts. Addressing these disparities requires targeted interventions and policy changes, emphasizing the need for equitable healthcare access and comprehensive support systems tailored to various communities. As the data continues to evolve, it is essential to advocate for improvements that could help reduce these distressing trends.
Understanding Preventable Pregnancy Deaths
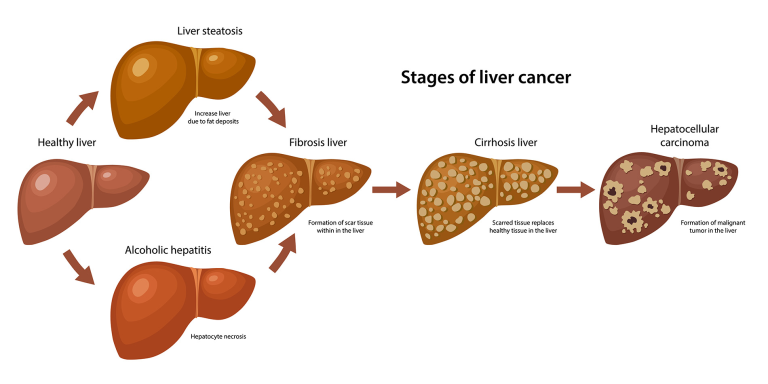
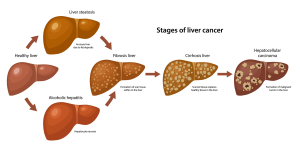
Preventable pregnancy deaths are a significant concern within maternal health discussions, warranting deeper analysis of underlying factors. The leading causes of maternal deaths are often linked to chronic conditions exacerbated during pregnancy, such as cardiovascular disease and hypertension. These chronic conditions, now affecting younger populations, highlight a shift in maternal health risks that demand urgent attention. Improving awareness and management of these conditions through prenatal education and healthcare accessibility is crucial in preventing unnecessary fatalities.
In addition to chronic conditions, the healthcare infrastructure plays a pivotal role in addressing the epidemic of preventable pregnancy deaths. The fragmented nature of the U.S. healthcare system often results in gaps in care, leading to inadequate monitoring and follow-up on high-risk pregnancies. Enhanced training for healthcare providers, as well as the implementation of national guidelines addressing maternal health, could streamline care processes and foster better health outcomes. Innovations in telemedicine and extended postpartum care services may also contribute to reducing the number of preventable deaths.
The Importance of Extended Postpartum Care
Extended postpartum care is critical for maternal health, especially considering that nearly one-third of pregnancy-related deaths occur between 42 days and one year after childbirth. Historically, the healthcare system has focused predominantly on the prenatal phase and the immediate postpartum period, often neglecting the ongoing recovery that many individuals experience. Studies suggest that by extending postpartum care, healthcare providers can monitor and address complications that arise after childbirth, thereby improving overall maternal health outcomes.
The need for a redefinition of postpartum care is underscored by the recognition that the postpartum period should be treated as a continuum rather than a fixed timeframe. Comprehensive postpartum care programs could significantly decrease late maternal deaths by ensuring that new mothers receive necessary support and interventions throughout their recovery. Enhanced education on postpartum health issues, coupled with better access to healthcare services, can foster recovery and well-being, ultimately leading to stronger maternal health metrics.
Racial Disparities in Maternal Health Outcomes
Racial disparities in maternal health remain a pressing issue in the U.S., with certain groups experiencing significantly higher mortality rates. Data consistently reveal that American Indian and Alaska Native women, as well as non-Hispanic Black women, face markedly increased risks of pregnancy-related deaths compared to their white counterparts. Structural inequities within the healthcare system, including access to quality care and implicit biases among medical professionals, contribute to these disparities and highlight the urgent need for policy reforms aimed at equitable healthcare.
Mitigating these disparities requires a multifaceted approach that includes community-centered initiatives and education tailored to the unique needs of different racial and ethnic populations. Innovative programs, such as those that foster collaboration between public health and community organizations, have the potential to effectively bridge the gap in maternal health care access. By investing in initiatives designed to address these systemic inequalities, stakeholders can work towards improving health outcomes for all pregnant individuals, thereby creating a more equitable healthcare landscape.
Addressing Chronic Conditions in Pregnancy
Chronic conditions during pregnancy pose significant risks, with increasing rates of hypertension and cardiovascular disease among expecting mothers. The alarming trend of younger women experiencing these health issues necessitates a reevaluation of maternal healthcare practices. Effective management of chronic conditions is essential throughout pregnancy to mitigate associated risks, including pregnancy-related deaths. Healthcare providers must prioritize screening and early intervention for pregnant individuals with preexisting conditions to help ensure safer pregnancies and deliveries.
Moreover, comprehensive education on chronic conditions must be a foundational aspect of prenatal care. By empowering individuals with knowledge about managing their health conditions before and during pregnancy, healthcare systems can potentially reduce the incidence of complications. Strategies such as personalized care plans and multidisciplinary support teams can foster better health outcomes for expectant mothers, leading to a decrease in both maternal mortality rates and associated healthcare costs.
Impact of Public Health Infrastructure on Maternal Health
The current state of public health infrastructure in the U.S. is a significant factor influencing maternal health outcomes. As investment in public health has faced cuts, tracking and addressing pregnancy-related deaths has become increasingly challenging. Only through robust and sustained funding can the public health system effectively monitor maternal health statistics and implement necessary interventions. Advocating for continued investment in public health infrastructure is vital for the improvement of maternal health outcomes and the reduction of pregnancy-related deaths.
Building an effective maternal health strategy requires a cohesive infrastructure that integrates various components of healthcare delivery. Policymakers should prioritize strengthening public health initiatives that enhance maternal care quality, from prenatal to extended postpartum support. This includes addressing disparities across states and ensuring consistency in the provision of maternal health services. By reinforcing public health infrastructure, the U.S. can better respond to the maternal health crisis and work towards achieving a significant reduction in pregnancy-related deaths.
The Role of Policy in Maternal Health Outcomes
Healthcare policy plays a crucial role in shaping maternal health outcomes and addressing maternal mortality rates. Variations in state policies often lead to unequal access to care, exacerbating the existing racial and economic disparities in maternal health. Policymakers must identify and implement evidence-based practices that support maternal health, such as expanding Medicaid coverage for pregnant individuals and improving access to comprehensive postpartum care.
Furthermore, targeted policies aimed at reducing healthcare inequities can create a more favorable environment for pregnant individuals. By fostering collaboration between public health organizations, healthcare providers, and community leaders, it is possible to develop initiatives that effectively address the needs of diverse populations. Advocacy for policy reforms that ensure equitable access to quality maternal healthcare is essential for achieving better health outcomes and reducing pregnancy-related deaths in the U.S.
The Need for Research and Data Tracking in Maternal Health
Ongoing research and effective data tracking are essential components of improving maternal health outcomes. The U.S. only recently implemented a national system for tracking maternal deaths through the pregnancy checkbox on death certificates, highlighting a significant gap in data collection prior to 2018. Consistent and comprehensive data tracking allows researchers and policymakers to identify trends, allocate resources effectively, and inform strategies for improving maternal care.
Increased funding for maternal health research is also critical for understanding the multifaceted issues contributing to pregnancy-related deaths. Without adequate research resources, efforts to improve maternal health outcomes may falter. Emphasizing the importance of data-driven decision-making in policy formulation can lead to innovative approaches that ultimately enhance the quality of maternal care and reduce disparities within the healthcare system.
Telemedicine’s Role in Maternal Health Care
Telemedicine has emerged as a vital tool in maternal healthcare, particularly in light of the challenges posed by the COVID-19 pandemic. With the rise of remote consultations, healthcare providers can reach pregnant individuals who may have difficulty accessing in-person care due to geographical or socioeconomic barriers. Telehealth services offer a convenient platform for discussing prenatal concerns, managing chronic conditions, and providing postpartum support, ultimately aiming to enhance maternal health outcomes.
Nevertheless, while telemedicine presents opportunities for improving access to maternal healthcare, it is essential to ensure that digital equity is prioritized. Disparities in access to technology and internet services can hinder the effectiveness of telehealth initiatives for certain populations. To maximize the potential of telemedicine in maternal care, stakeholders must address these gaps and advocate for policies that facilitate inclusive access to virtual healthcare services for all pregnant individuals.
Frequently Asked Questions
What are the current trends in pregnancy-related deaths in the U.S.?
Pregnancy-related deaths in the U.S. have been steadily rising, particularly between 2018 and 2022. In 2022, the maternal mortality rate reached 32.6 deaths per 100,000 live births, up from 25.3 in 2018. The increase has been attributed to various factors including chronic conditions in pregnancy, inadequate postpartum care, and systemic racial disparities in maternal health.
What are the main causes of preventable pregnancy deaths in the U.S.?
Over 80% of pregnancy-related deaths in the U.S. are deemed preventable. The leading cause is cardiovascular disease, which includes hypertension and complications like pre-eclampsia. Other significant contributors include delayed access to care, lack of proper postpartum support, and healthcare disparities affecting marginalized racial groups.
How do racial disparities impact maternal mortality rates in the U.S.?
Racial disparities play a critical role in maternal mortality rates in the U.S. For instance, American Indian and Alaska Native women face a mortality rate of 106.3 deaths per 100,000 live births, nearly four times that of white women, who have a rate of 27.6. These disparities are exacerbated by systemic bias and inequitable healthcare access.
Why is postpartum care vital in reducing pregnancy-related deaths?
Postpartum care is essential in preventing pregnancy-related deaths as nearly one-third of these deaths occur between 42 days and one year after delivery. Improved healthcare systems that extend support during the postpartum period could significantly reduce late maternal deaths and improve overall maternal health outcomes.
What are some interventions to address chronic conditions in pregnancy?
Interventions to address chronic conditions in pregnancy include better screening and management of conditions like hypertension and diabetes before and during pregnancy, increased access to comprehensive prenatal care, and continuous monitoring throughout the pregnancy and postpartum period to address complications early.
What steps can be taken to lower maternal mortality rates across different states in the U.S.?
To lower maternal mortality rates, states can invest in maternal health programs, improve healthcare access especially in rural areas, enforce equitable health policies, standardize care practices, and prioritize funding for maternal health research and public health infrastructure.
How significant is the impact of COVID-19 on pregnancy-related deaths?
The COVID-19 pandemic has likely influenced the rise in pregnancy-related deaths due to stress on healthcare systems, increased rates of chronic conditions, and challenges in accessing care. The data from the study indicates a sharp rate increase in 2021, which underscores the pandemic’s profound impact on maternal health.
What role does public health infrastructure play in maternal health outcomes?
Public health infrastructure is crucial for improving maternal health outcomes in the U.S. A strong infrastructure enables better tracking of maternal mortality data, facilitates access to necessary health services, and supports policy advocacy aimed at enhancing care for pregnant individuals, ultimately reducing pregnancy-related deaths.
| Key Points | Details |
|---|---|
| Rise in pregnancy-related deaths | Over 80% are preventable; U.S. has highest maternal mortality rate among high-income countries. |
| Data source and time frame | Study used CDC data spanning 2018-2022, noting a rise in deaths, particularly after the pandemic onset. |
| Racial disparities | American Indian/Alaska Native women have the highest mortality rate; disparities persist across racial groups. |
| Leading cause of death | Cardiovascular disease has now replaced hemorrhage as the leading cause of pregnancy-related deaths. |
| Late maternal deaths | Deaths occurring 42 days to 1 year after pregnancy should be included in mortality rates for a comprehensive view. |
| Need for improved healthcare systems | Investment in public health infrastructure is crucial to address rising rates and inequities. |
| Effective policy changes | Addressing state-level disparities and enhancing quality care is essential for improving maternal health outcomes. |
Summary
Pregnancy-related deaths in the U.S. continue to rise, highlighting a severe public health crisis. Despite 80% being preventable, the U.S. exhibits the highest maternal mortality rate among wealthy nations. Disparities among racial and ethnic groups contribute significantly to these figures, with urgent calls for improved healthcare access and systemic changes. Without proper investment in public health infrastructure and innovative maternal care solutions, the trend of increasing pregnancy-related deaths may persist, emphasizing the need for nationwide awareness and action.