Pediatric cancer recurrence remains a critical concern for healthcare providers, especially in the context of childhood brain tumors like gliomas. Recent advancements involving AI in medicine have shed light on predicting cancer relapse with improved precision, significantly benefiting young patients. Research has demonstrated that employing MRI brain scans analyzed through temporal learning in AI can enhance relapse prediction accuracy, moving beyond traditional methods that often fall short. Such innovations are essential as many pediatric gliomas, despite being treatable, carry the harsh reality of possible recurrence, necessitating expansive follow-up care. By integrating these advanced technologies, medical practitioners hope to not only mitigate stress for patients and their families but also enhance treatment outcomes for those facing this daunting diagnosis.
In the realm of childhood oncology, the re-emergence of cancer, often termed pediatric oncology relapse, becomes a pressing issue for both patients and caregivers. As researchers delve into the role of artificial intelligence tools within clinical settings, the importance of understanding how children’s tumor types, particularly brain tumors, respond to treatments has never been more clear. Enhanced imaging techniques, including serial brain imaging assessments, enable clinicians to gather comprehensive data over time, fueling better predictive models for identifying those at risk of cancer resurgence. Innovations in technology, such as sophisticated AI algorithms that analyze patterns in imaging studies, are paving the way for tailored therapeutic strategies. This pursuit emphasizes the necessity for continuous research and development to alleviate the burden linked to pediatric oncologic conditions.
Advancements in AI for Predicting Pediatric Cancer Recurrence
Artificial intelligence (AI) is transforming the landscape of pediatric healthcare by enhancing the predictive capabilities of cancer relapse. In recent studies, AI tools have demonstrated remarkable proficiency in analyzing numerous brain scans over time, significantly improving the accuracy of pediatric cancer recurrence predictions compared to traditional methods that rely on single images. The ability to leverage large datasets, such as those gathered from nearly 4,000 MRI brain scans, has enabled researchers to create sophisticated models capable of identifying subtle changes indicative of relapse in pediatric gliomas.
These advancements are particularly crucial in the management of pediatric gliomas, which, while often treatable, can lead to devastating outcomes when recurrence occurs. As noted by researchers, relying solely on frequent follow-up imaging can create stress and anxiety for both patients and their families. By integrating AI into clinical practices, there is hope for a more precise identification of high-risk patients, potentially minimizing unnecessary imaging and allowing for timely intervention.
The Role of Temporal Learning in Cancer Relapse Prediction
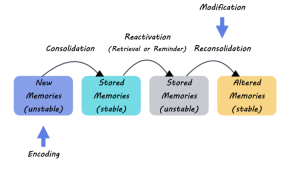
Temporal learning is an innovative approach that stands at the forefront of AI applications in medicine, particularly in predicting cancer relapse. By training AI models to consider sequences of MRI scans taken over time, researchers can capture the temporal dynamics of gliomas more effectively. This method contrasts sharply with traditional AI models that predominantly analyze single images, thus enhancing the ability to make informed predictions about a patient’s likelihood of recurrence after surgery.
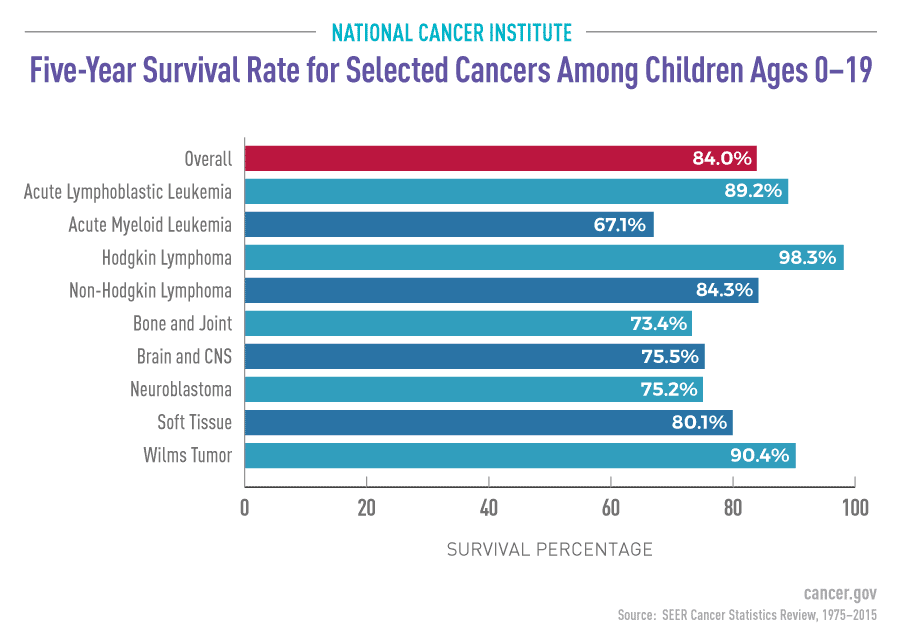
The findings from the Mass General Brigham study reveal that employing temporal learning has dramatically improved prediction accuracy, soaring to between 75-89% within one year post-treatment. This represents a significant advancement over previous predictions based on individual scans, which had accuracy rates hovering around 50%. By utilizing multiple data points, temporal learning creates a more nuanced understanding of disease progression, offering the potential for tailored treatment strategies that could drastically improve outcomes for pediatric patients.
Implementing AI in MRI Brain Scans for Pediatric Patients
The integration of AI into MRI brain scan protocols signifies a paradigm shift in pediatric oncology. Traditional imaging approaches often focus on static assessments at single points in time, risking missed opportunities for early intervention. The AI tools utilized in current research provide real-time analysis of sequential brain scans, allowing healthcare providers to detect and address clinical changes as they arise. This continuous monitoring is particularly critical for pediatric gliomas, which can vary drastically in terms of recurrence risk.
Furthermore, by analyzing patterns across multiple scans, AI can inform decisions on when to reduce imaging frequencies for lower-risk patients or initiate preemptive treatments for those identified as high-risk. This not only optimizes resource utilization but also reduces the emotional and logistical burden on families. As the use of AI becomes more widespread, it has the potential to redefine standard protocols in pediatric care, leading to earlier and more effective interventions.
Challenges and Considerations in AI Application for Pediatric Cancer
Despite the promise of AI in predicting pediatric cancer recurrence, challenges remain in its clinical application. One primary concern is the need for extensive validation across diverse patient populations to ensure the reliability of AI-driven predictions. The initial findings from studies highlight significant accuracy, but without further cross-institution verification, the transition from research to routine practice may encounter significant hurdles.
Additionally, ethical considerations surrounding patient data privacy and consent must be carefully navigated as AI systems rely heavily on large datasets. Parents and guardians may have concerns about the implications of AI in their child’s care, necessitating transparent communication about how their health information is used and the potential benefits of AI-driven insights. Engaging families in the conversation around AI and its applications can help build trust and understanding as these technologies develop.
The Future of Pediatric Cancer Treatment with AI
The future of pediatric cancer treatment is likely to be markedly influenced by advancements in AI technology. As researchers refine AI tools that can analyze complex patterns in medical imaging, the potential for personalized medicine in pediatric oncology will only expand. Innovations such as the temporal learning model serve as a blueprint for how AI can be harnessed to predict cancer relapse, thus paving the way for more nuanced and effective treatment plans tailored to individual patient needs.
Furthermore, ongoing clinical trials and research will provide vital insights into the efficacy of AI in real-world settings, shaping the protocols for pediatric cancer treatment. By integrating the predictive capabilities of AI with existing treatment options, healthcare providers can move towards a more proactive approach that not only treats cancer but also anticipates its challenges, ultimately fostering a more hopeful prognosis for young patients and their families.
Enhancing Family Support Through AI in Oncology
The integration of AI technology in pediatric oncology extends beyond medical outcomes to include emotional and psychological support for families. Early prediction of pediatric cancer recurrence can significantly alleviate stress and anxiety for both patients and their families. By employing advanced AI models, healthcare providers can offer more personalized care approaches, which include tailored follow-up plans and counseling based on the projected risk assessment.
Moreover, understanding when families can expect follow-up imaging can help them prepare mentally and logistically. By reducing the uncertainty and potential for false alarms through more accurate AI models, families can focus on what matters most: their child’s quality of life. Enhancing family support through these technological advancements fosters a collaborative environment where families can become partners in the care process.
AI as a Tool for Educating Patients and Families
Incorporating AI into pediatric oncology not only aids in clinical predictions but also serves as an educational tool for patients and their families. Clear, accessible information about the role of AI in predicting pediatric cancer recurrence can empower families to make informed decisions about treatment options. Providing resources that explain how AI analyzes medical data, such as MRI scans, can demystify the technology and promote understanding of its benefits and limitations.
Furthermore, workshops or informational sessions led by healthcare teams can enhance engagement and support for families navigating cancer care. When patients and their families have a comprehensive understanding of how AI supports personalized treatment plans, it can foster a more collaborative relationship with their medical teams. This empowerment aspect is vital, as it creates a proactive patient community that actively participates in the cancer care journey.
The Intersection of AI and Research in Pediatric Oncology
As AI continues to evolve, its impact on research within the field of pediatric oncology is profound. The ability to analyze vast amounts of medical imaging data opens new horizons for clinical studies, allowing researchers to investigate correlations between treatment responses and imaging biomarkers. This intersection of AI and research can lead to the development of groundbreaking therapeutic strategies tailored specifically for the pediatric population.
Moreover, the collaboration between institutions, such as the partnerships formed during the Harvard study, emphasizes the importance of a collective approach in advancing pediatric oncology. By pooling resources and expertise, researchers can expedite the development and validation of AI models, ultimately leading to innovative solutions that improve patient outcomes and reduce the burden of pediatric cancer.
Clinical Trials and the Future of AI in Pediatric Oncology
The pathway to integrating AI into pediatric oncology involves conducting clinical trials that assess the efficacy of AI-driven predictions in real-world settings. These trials will provide critical data on how well AI models can perform in diverse populations, as well as their potential to improve patient management strategies. Additionally, understanding the outcomes of AI-informed care could illuminate the benefits of reducing unnecessary imaging and focusing interventions on high-risk patients.
As the field progresses, the outcomes of ongoing trials will serve as a benchmark for future AI applications in medicine. The hope is that successful implementation of AI-assisted predictions will not only fulfill clinical needs but also contribute to the overall enhancement of healthcare systems in managing pediatric cancer, thus ensuring that every child receives the most effective care possible.
Frequently Asked Questions
What are the key factors influencing pediatric cancer recurrence in gliomas?
Pediatric cancer recurrence, particularly in gliomas, is influenced by factors including tumor grade, surgical margins, and the presence of residual disease. Treatment protocols and genetic markers also play significant roles in determining relapse risk.
How does AI improve the prediction of pediatric cancer recurrence?
AI enhances the prediction of pediatric cancer recurrence by analyzing multiple MRI brain scans over time. This temporal learning approach allows the AI model to identify subtle changes indicative of relapse, improving accuracy significantly beyond traditional single-scan methods.
What role do MRI brain scans play in assessing pediatric cancer recurrence?
MRI brain scans are crucial for monitoring pediatric cancer recurrence as they provide real-time insights into a patient’s brain health post-treatment. Frequent imaging helps track potential relapses, but advancements in AI are making this process more efficient and less burdensome for families.
Can temporal learning in AI effectively predict cancer relapse in pediatric patients?
Yes, temporal learning in AI has shown promise in predicting cancer relapse in pediatric patients with gliomas. By analyzing sequential MRI brain scans, this method increases accuracy in identifying relapse risk, offering hope for better management of pediatric cancer recurrence.
What advancements have been made in predicting pediatric cancer recurrence?
Recent advancements include the development of AI tools that use temporal learning techniques to analyze MRI brain scans over time, drastically improving relapse prediction accuracy for pediatric gliomas compared to traditional methods.
Why is identifying pediatric cancer recurrence early important?
Identifying pediatric cancer recurrence early is vital as it allows for timely intervention and treatment adjustments, which can improve outcomes. Many pediatric gliomas, though treatable, can lead to severe consequences if not detected early.
What is the future of AI in predicting pediatric cancer recurrence?
The future of AI in predicting pediatric cancer recurrence looks promising, with ongoing research aimed at validating AI models for broader clinical application. Optimizing imaging frequency and targeted therapies based on AI predictions could revolutionize care for pediatric glioma patients.
How does the accuracy of AI predictions compare to traditional methods for pediatric cancer recurrence?
AI predictions for pediatric cancer recurrence using temporal learning have shown accuracy rates between 75-89%, which is significantly higher than the approximately 50% accuracy of traditional single-image analysis methods.
| Key Points | Details |
|---|---|
| AI Tool for Recurrence Prediction | An AI system outperformed traditional methods in predicting relapse risk for pediatric glioma patients. |
| Research Details | Study involved nearly 4,000 MR scans from 715 pediatric patients, published in NEJM AI. |
| Temporal Learning Technique | Innovative use of multiple scans over time for better prediction accuracy. |
| Prediction Accuracy | 75-89% accuracy for glioma recurrence one year post-treatment. |
| Clinical Implications | Potential to reduce stress and frequency of MRIs for low-risk patients, and improve targeting for high-risk patients. |
Summary
Pediatric cancer recurrence is a significant concern, particularly for those diagnosed with gliomas. Recent advancements in AI technology have proven to effectively predict the risk of recurrence, providing a promising pathway toward better management of pediatric brain tumors. The study highlights the urgent need for improved diagnostic tools to identify at-risk patients early, potentially transforming care approaches for children facing this devastating disease.