AI in pediatric brain cancer is revolutionizing the way we understand and manage this challenging disease. Recent advancements have shown that AI tools analyzing multiple brain scans can predict relapse risk in children with brain tumors, specifically pediatric gliomas, with unprecedented accuracy. Traditional methods often fall short, leaving families anxious and children undergoing numerous imaging tests, yet AI cancer prediction models are changing this landscape. By employing a technique known as temporal learning in medicine, researchers are able to train AI systems to detect subtle changes in brain scans over time, enhancing their predictive capabilities. This innovative approach not only aims to improve accuracy in identifying recurrence risk in children but also holds promise for transforming the care and treatment of pediatric brain cancer patients.
The emergence of artificial intelligence in the field of pediatric oncology is paving new pathways for understanding how to combat brain cancer in children. Utilizing advanced algorithms, researchers are developing predictive models that assess the likelihood of recurrence in pediatric gliomas, which poses a significant challenge in clinical practice. By leveraging vast datasets of medical imaging over time, these tools can analyze intricate patterns that may go unnoticed by human eyes, further enhancing AI cancer prediction efforts. This methodology employs strategies analogous to temporal assessments, allowing healthcare practitioners to make informed decisions about patient treatment plans. As the research progresses, the potential for better management of recurrence risk in children suffering from brain tumors becomes an increasingly tangible reality.
Introduction to Pediatric Brain Cancer
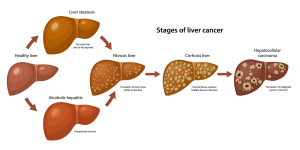
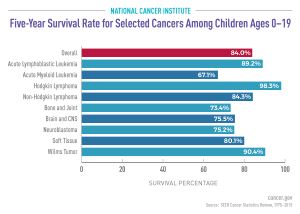
Pediatric brain cancer is a significant health concern, with gliomas being one of the most common types affecting children. These tumors originate in the brain and can vary widely in terms of aggressiveness and treatment options. Understanding the nature and treatment of pediatric gliomas is crucial for timely intervention, as early detection can lead to more effective management and improved survival rates. With advancements in technology, healthcare providers are increasingly leveraging modern tools to enhance diagnosis and treatment.
Unfortunately, the journey through treatment and recovery for children with brain cancer can be fraught with challenges. The emotional toll on families, coupled with the physical burdens of frequent hospital visits and imaging tests, can become overwhelming. Hence, there is a pressing need for innovative approaches that ease these burdens while enhancing care quality for children diagnosed with brain tumors.
Advancements in AI for Pediatric Gliomas
Recent advancements in artificial intelligence (AI) are proving to be game changers in the field of pediatric oncology. Specifically, researchers at Mass General Brigham have developed an AI tool that can analyze longitudinal brain scans and predict the risk of relapse in pediatric cancer patients more reliably than traditional methods. This AI-driven approach represents a shift away from relying solely on single imaging assessments, which often fall short of accurately forecasting recurrence risks.
The introduction of temporal learning in medical imaging allows the AI to evaluate multiple scans over time, enhancing its prediction capabilities. By teaching the model to recognize the changes in the brain images collected post-surgery, the AI can identify patterns that indicate potential cancer recurrence much earlier. This approach offers hope for improving clinical outcomes and reducing the anxiety for young patients and their families associated with prolonged follow-up imaging.
Understanding Recurrence Risk in Children with Brain Cancer
The risk of recurrence in children diagnosed with brain cancer presents a significant challenge for doctors and families alike. The treatment landscape for pediatric gliomas is complex, as some tumors are more prone to returning than others. Thus, distinguishing between low and high-risk patients is essential for tailoring personalized treatment plans. Studies show that relapses can lead to devastating consequences for young patients, reaffirming the importance of accurate risk assessment.
With the integration of AI technologies, healthcare providers can now better predict recurrence in pediatric brain cancer patients. The predictive accuracy achieved through temporal learning—between 75-89%—marks a remarkable improvement over traditional methods. By focusing on the dynamic changes occurring in a child’s brain during the post-treatment phase, doctors can respond proactively, potentially altering the course of treatment before the cancer recurs, significantly improving survivorship outcomes.
The Role of AI in Cancer Prediction
AI cancer prediction tools are revolutionizing the landscape of oncology, with a promise of more accurate diagnostics and personalized care. By analyzing vast datasets from diverse patient populations, AI models like the one developed at Mass General Brigham can discern complex patterns and trends that would be imperceptible to human observers. This technology signifies a major advancement in the precision of cancer predictions, allowing clinicians to make enhanced informed decisions.
In pediatric cases, where the stakes are particularly high, such predictive capabilities can reshape treatment paradigms. Used effectively, AI can significantly decrease the frequency of invasive imaging for low-risk patients and introduce more aggressive monitoring or treatments for those identified at higher risk of recurrence. This proactive approach aims to improve overall treatment efficacy and patient comfort during recovery.
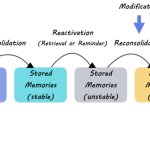
Temporal Learning in Medicine
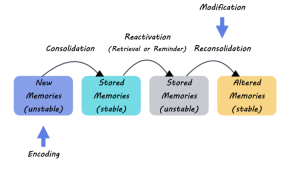
The application of temporal learning within AI models is a relatively new but promising methodology in the realm of medicine. By utilizing a chronological sequence of medical images, researchers can train AI to observe and learn from the subtle changes in a child’s brain over time. This method contrasts sharply with traditional models that typically analyze individual scans without accounting for the progress or regression of brain conditions.
Temporal learning not only enhances prediction accuracy but also fosters a deeper understanding of disease progression. In the context of pediatric brain cancer, it allows for a tailored approach to patient management, where clinicians can gauge the evolution of a tumor with confidence. Enhanced monitoring driven by AI insights can lead to more timely interventions, ultimately aiming to prevent relapses and improve treatment outcomes.
Reducing Stress for Patients and Families
The emotional impact of a pediatric brain cancer diagnosis extends beyond the child’s physical health; it permeates the entire family dynamic. Every imaging appointment and hospital visit can heighten anxiety levels for both children and their caregivers, leading to significant emotional strain. Innovations like AI-driven predictive models aim to alleviate some of this stress by reducing unnecessary imaging for low-risk patients and streamlining care plans.
Through better prediction of recurrence risks and tailored follow-up protocols, families can experience less turmoil during what can be an exceptionally challenging period. As these AI tools become more integrated into clinical practice, they may offer a newfound sense of control to families, resulting in improved patient experiences and outcomes in the treatment of pediatric brain cancer.
Future Directions in Pediatric Oncology
The future of pediatric oncology is poised for transformation, with AI at the forefront driving enhancements in patient care. As research continues to validate the efficacy of tools leveraging temporal learning and predictive analytics, clinical trials will play a pivotal role in assessing their integration into routine practice. The objective is to refine care pathways while ensuring that young patients receive the most optimal treatment based on their individual risk profiles.
Looking ahead, we can expect broader collaboration among academic institutions, healthcare providers, and technology developers to further progress in this vital field. With a collective focus on harnessing AI’s potential, the hope is to significantly reduce the burden of brain cancer in children, ultimately paving the way for a future where early intervention and precision medicine become the norm.
Collaboration and Innovation in Pediatric Cancer Research
Collaboration among research institutions is crucial for advancing the fight against pediatric brain tumors. The research conducted by Mass General Brigham, Boston Children’s Hospital, and Dana-Farber/Boston Children’s Cancer and Blood Disorders Center illustrates the power of partnerships in uncovering novel insights into the complexities of pediatric oncology. By pooling resources and expertise, these institutions can foster innovation and expedite research outcomes.
Furthermore, the collaboration facilitates the development of cutting-edge technologies, such as AI-based predictive models, which can have profound implications on patient care. Such innovations not only enhance the precision of treatment for pediatric gliomas—including better predictions of recurrence risk—but also contribute to a healthier collaboration ecosystem that prioritizes patient welfare and scientific discovery.
The Importance of Early Detection in Brain Cancer Among Children
Early detection of pediatric brain cancer is paramount to improving survival rates and reducing long-term complications. Timely intervention can make a critical difference, especially when it comes to treating gliomas that may otherwise relapse. Innovative monitoring techniques, alongside AI advancements, play a vital role in identifying these conditions early, enabling healthcare professionals to begin treatment at the most opportune moment.
Given the often atypical presentation of brain tumors in children, having advanced tools that enhance diagnostic capabilities allows for a more precise and proactive healthcare approach. AI-driven predictions combined with comprehensive monitoring present a promising future where the chances of successful treatment and long-term health are significantly improved for children facing brain cancer.
Frequently Asked Questions
What role does AI play in the prediction of pediatric gliomas recurrence risk?
AI plays a significant role in predicting the recurrence risk of pediatric gliomas by analyzing multiple brain scans over time, leading to more accurate predictions compared to traditional imaging methods. This advanced approach allows for identification of subtle changes in brain scans, resulting in improved outcomes for children diagnosed with brain cancer.
How does AI enhance the management of brain cancer in children?
AI enhances the management of brain cancer in children by facilitating the accurate prediction of relapse through temporal learning techniques that utilize serial imaging. This allows healthcare providers to monitor high-risk patients more effectively and potentially reduce the frequency of follow-up imaging for lower-risk cases.
What is temporal learning in medicine, and how does it apply to pediatric brain cancer?
Temporal learning in medicine refers to the method of training AI models using sequences of data collected over time, such as consecutive brain scans of pediatric patients after surgery. This technique significantly improves the AI’s ability to predict the recurrence of pediatric brain cancer by capturing gradual changes in tumors.
What improvements have AI tools made in predicting relapse risk in pediatric brain cancer patients?
AI tools have improved the prediction of relapse risk in pediatric brain cancer patients by achieving an accuracy rate of 75-89%, compared to approximately 50% with traditional single-scan methods. This advancement allows for better-informed decisions regarding follow-up care and treatment.
Can AI be used to reduce anxiety in children with brain cancer by predicting recurrence?
Yes, AI can help reduce anxiety in children with brain cancer by providing more accurate predictions about recurrence risks, thus minimizing unnecessary imaging procedures and associated stress for patients and their families. This proactive approach allows clinicians to tailor follow-up care based on individual risk assessments.
What are the future implications of AI in the treatment of pediatric gliomas?
The future implications of AI in the treatment of pediatric gliomas include the potential for personalized treatment plans based on accurate risk predictions, the possibility of launching clinical trials, and redefining follow-up imaging protocols. These advancements aim to enhance patient care and outcomes in children dealing with brain cancer.
How does AI cancer prediction technology work for pediatric brain cancer?
AI cancer prediction technology for pediatric brain cancer works by analyzing longitudinal MRI scans to detect changes over time, employing models trained to identify patterns associated with tumor recurrence. This method allows for early intervention in cases deemed high-risk, leading to tailored treatment strategies.
What is the significance of AI’s ability to analyze multiple MRIs for pediatric brain cancer?
The significance of AI’s ability to analyze multiple MRIs lies in its enhanced predictive power for recurrence, enabling the identification of subtle tumor changes over time rather than relying on single images. This marks a crucial advancement in managing pediatric gliomas and improving patient outcomes.
| Key Points | Details |
|---|---|
| AI Tool Prediction | An AI tool predicts relapse risk in pediatric brain cancer more accurately than traditional methods. |
| Study Significance | The study could lead to improved care for children with gliomas and reduce stress from frequent imaging. |
| Techniques Used | Temporal learning allows the AI to analyze multiple scans over time for better accuracy. |
| Prediction Accuracy | The AI predicted recurrence with 75-89% accuracy, better than the 50% accuracy of single image assessments. |
| Future Directions | Further validation and clinical trials are planned to improve patient care through AI-informed predictions. |
Summary
AI in pediatric brain cancer is proving to be a game-changer in the fight against this devastating disease. By training advanced AI models with temporal learning, researchers are able to harness data from multiple brain scans, improving prediction accuracy for relapse risk in pediatric gliomas. This innovative technique not only enhances the ability to identify high-risk patients early but also reduces the emotional and logistical burdens associated with frequent MRI scans. As the research evolves, the hope is to translate these findings into clinical practice, ultimately improving outcomes and quality of life for young cancer patients.