Pediatric cancer recurrence presents significant challenges for patients and families alike, especially in cases involving brain tumors like gliomas. Recent advancements in AI tools offer new hope, as studies show these sophisticated systems outperform traditional methods in predicting the risk of relapse in young patients. By analyzing a series of brain scans, these algorithms provide insights that guide treatment plans, potentially reducing emotional burden and stress associated with repetitive imaging. Furthermore, this leap in technology aligns with the Department of Radiation Oncology’s ongoing research efforts, highlighting the importance of machine learning in medicine. As pediatric glioma research continues to evolve, integrating AI-based predictions into clinical practices may revolutionize the management of brain cancer relapse in children.
The recurrence of childhood cancer, particularly in the context of brain tumors, remains a pressing concern for healthcare providers and caretakers. Terms such as pediatric cancer relapse, glioma recurrence, and brain tumor re-emergence illustrate the serious implications of such conditions on young patients. Innovative research utilizing artificial intelligence has emerged as a promising avenue, enhancing our understanding and prediction capabilities surrounding these occurrences. As medical professionals explore the intersection of machine learning and pediatric oncology, they aim to offer more personalized treatment strategies. This shift in approach not only aims to alleviate the stress on families but also strives to improve overall patient outcomes in cases of childhood brain tumors.
Understanding Pediatric Cancer Recurrence
Pediatric cancer recurrence poses significant challenges for clinicians and families alike. In particular, brain tumors like gliomas have unique pathways to recurrence, making early detection of relapse critical for improving patient outcomes. Many treatments, including surgery, can initially be effective, but the risk of recurrence remains a haunting reality for many families. This underlines the importance of research, such as the recent findings published in The New England Journal of Medicine AI, which illustrate how advanced tools like AI can transform our approach to monitoring these patients.
Researchers stress that with innovations in medical imaging and machine learning, predicting which pediatric patients are at greatest risk for cancer recurrence can become more accurate. This enables healthcare providers to tailor follow-up protocols and make informed decisions on the necessity and frequency of imaging. For instance, employing AI tools that analyze longitudinal data from multiple MRIs equips physicians with insights that traditional methods lack, thereby mitigating the emotional and physical burden associated with frequent imaging.
The Role of AI in Pediatric Oncology
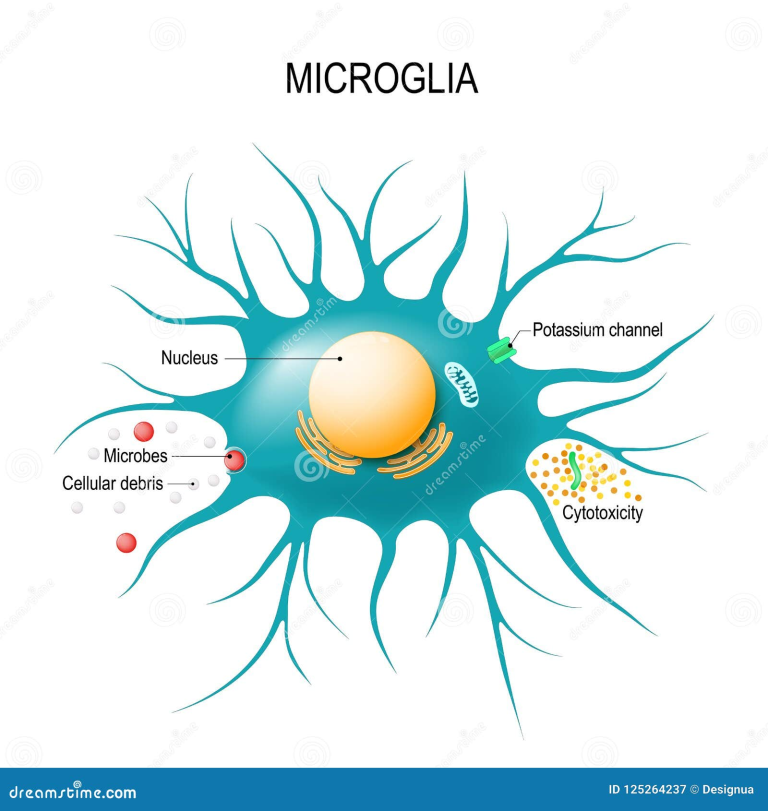
Artificial Intelligence (AI) is revolutionizing pediatric oncology, notably in predicting treatment outcomes and recurrence rates in children with cancer. The application of machine learning algorithms, as seen in Mass General Brigham’s recent study, shows promise in enhancing predictive accuracy for glioma treatment. By analyzing multiple images over time, AI not only improves the understanding of disease progression but also helps clinicians to identify patterns that can aid in developing personalized treatment plans.
The integration of AI into pediatric oncology signifies a paradigm shift in how cancer care is delivered. With traditional methods often relying on static, single-image analyses, AI offers a dynamic approach to interpreting temporal data from scans. This advancement not only signifies improved accuracy in identifying at-risk patients but also enhances the overall treatment framework, paving the way for potential innovations in targeted therapies and management strategies.
Glioma Treatment Prediction: A New Frontier
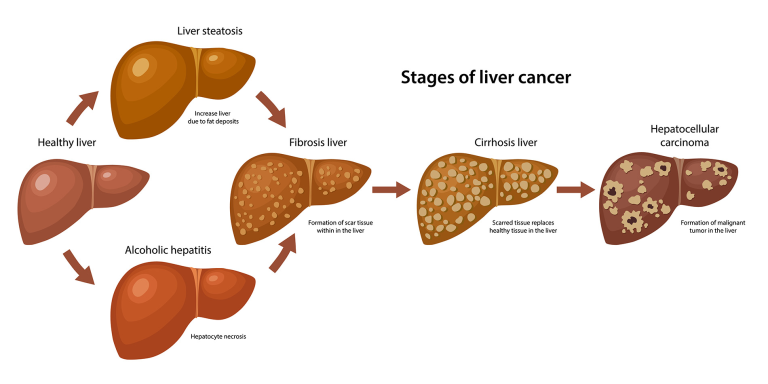
Gliomas, a common type of brain tumor among children, are notoriously difficult to manage due to their variable nature and the potential for recurrence after treatment. Recent studies have indicated that advancements in machine learning may play a vital role in predicting glioma treatment outcomes. With the ability to analyze sequential imaging data, AI tools can offer insights into how gliomas respond to therapies over time, which can be crucial for determining the next steps in a child’s treatment journey.
As pediatric glioma research continues to evolve, the deployment of AI in predicting treatment responses may not only enhance survival rates but also improve the quality of life for young patients. Early identification of treatment effectiveness enables healthcare providers to pivot their strategies promptly, reducing the chances of relapse and addressing issues before they escalate. Innovations in predictive modeling represent just the beginning of what technology can achieve in managing complex pediatric cancers.
Machine Learning in Medicine: Transforming Cancer Care
Machine learning stands at the forefront of transforming cancer care, particularly in pediatrics. In cases of pediatric gliomas, machine learning algorithms are utilized to enhance the understanding of disease patterns based on historical and real-time data. The ability of AI to process vast amounts of imaging and clinical data allows for earlier detection of complications, such as tumor recurrence, and facilitates personalized care tailored to individual patient profiles.
The integration of machine learning with existing medical practices is reshaping how healthcare professionals approach treatment planning and decision-making. By leveraging predictive analytics, oncologists can optimize treatment regimens, potentially improving outcomes for children diagnosed with brain cancers. The promise of AI and machine learning in medicine is clear: by providing precise, data-driven insights, we can significantly elevate the standard of care for young cancer patients.
The Importance of Longitudinal Imaging in Pediatric Cancer
Longitudinal imaging is pivotal in the management of pediatric cancer, especially for detecting recurrence in cases like gliomas. This approach involves monitoring patients over time with multiple imaging studies, which provides a comprehensive view of tumor behavior post-treatment. By utilizing advanced AI algorithms to analyze these serial scans, clinicians can gain insights that were previously unattainable, allowing for timely interventions when necessary.
Furthermore, longitudinal imaging reduces ambiguity in monitoring treatment responses. With AI’s capability to identify subtle changes across multiple time points, healthcare providers can adopt a more proactive stance against the risk of relapse. This not only enhances patient safety but also contributes to optimizing the use of healthcare resources, ensuring that children receive necessary imaging without unnecessary stress or excessive procedures.
Reducing Stress for Families Through Predictive Tools
For families navigating the complexities of pediatric cancer, the emotional and psychological toll can be overwhelming, especially with the uncertainty of cancer recurrence looming. AI and machine learning tools that predict relapse risk provide a significant advantage in alleviating some of this stress. By offering clearer insights into a patient’s likelihood of recurrence, families can engage in more informed discussions with their healthcare team and make empowered decisions regarding their child’s care.
Additionally, as predictive tools become more reliable, the frequency of imaging procedures may be adjusted based on a child’s risk level. For instance, lower-risk patients could benefit from a reduction in the number of follow-up scans, which not only enhances the quality of life for young patients but also alleviates the anxiety associated with frequent hospital visits. This innovative approach to care underscores the importance of integrating technology in pediatric oncology to enhance both clinical outcomes and family well-being.
The Future of AI in Pediatric Glioma Management
The future of AI in managing pediatric gliomas holds immense potential, with ongoing research aiming to refine predictive models and enhance clinical applications. As more studies emerge, demonstrating the effectiveness of AI in predicting treatment outcomes, the focus will likely shift toward integrating these tools into standard clinical workflows. This could revolutionize how pediatric oncologists monitor their patients, making early intervention feasible and systematic.
Moreover, the continuous development of smarter algorithms that integrate diverse types of data—from genomic information to historical imaging—will further enhance precision medicine in pediatric oncology. These innovations not only promise to improve survival rates but also support the holistic care of children affected by cancer, ensuring that each child receives personalized, effective, and compassionate treatment.
Collaboration in Pediatric Cancer Research
Collaboration between research institutions, hospitals, and technological innovators is crucial for advancing pediatric cancer research. The recent findings on using AI for predicting pediatric cancer recurrence underscore the importance of partnerships, as seen in the study conducted by Mass General Brigham in collaboration with Boston Children’s Hospital and Dana-Farber/Boston Children’s Cancer and Blood Disorders Center. Such collaborations leverage diverse expertise and resources needed to tackle the complexities of childhood cancers, driving innovation forward.
Integrating AI in pediatric oncology is not solely a technical endeavor; it requires clinicians, researchers, and technology experts working together to translate findings into clinical practice. By fostering an environment of collaboration, we can accelerate the pace at which discoveries are implemented, ultimately leading to improved outcomes for children battling cancer. These partnerships will be vital in ensuring that the next generation of cancer therapies is informed by the latest technological advancements.
Implementing Clinical Trials for AI-based Predictive Models
Moving from research to real-world application, implementing clinical trials for AI-based predictive models in pediatric cancer is a necessary step to validate their effectiveness. The promise shown by the temporal learning models developed for glioma patients highlights the need for rigorous testing in varied clinical environments. These trials can reveal how AI-driven predictions can improve treatment protocols, patient safety, and overall care quality.
As researchers prepare to launch clinical trials aimed at assessing the real-world impact of AI predictions, the focus will be on determining not just accuracy, but also the practical implications for patient outcomes. These insights will be essential for building trust among clinicians and families in AI applications for pediatric oncology. By ensuring that these technologies are thoroughly evaluated, we can confidently integrate AI into care pathways and enhance the management of pediatric cancer patients.
Frequently Asked Questions
How does AI contribute to predicting pediatric cancer recurrence?
AI plays a significant role in predicting pediatric cancer recurrence by analyzing multiple brain scans over time, offering greater accuracy than traditional imaging methods. Research in pediatric oncology indicates that using AI, particularly through techniques like temporal learning, can identify subtle changes that may indicate relapse risks in conditions such as gliomas.
What are the implications of early warning systems for pediatric cancer recurrence?
Early warning systems for pediatric cancer recurrence are crucial as they can reduce unnecessary stress from frequent follow-up imaging and allow for timely interventions. Improved prediction models, such as those developed using AI in pediatric oncology, provide a clearer assessment of which patients may be at risk for brain cancer relapse, leading to more personalized care.
What is the accuracy rate of AI in predicting brain cancer relapse in children?
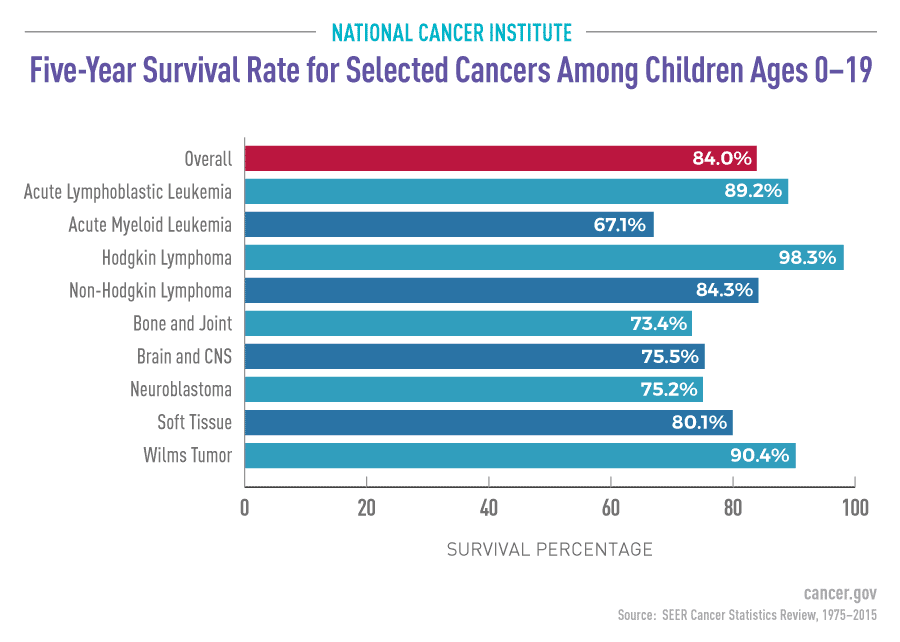
The AI model developed for predicting brain cancer relapse in pediatric patients has demonstrated an impressive accuracy rate of 75-89% in foreseeing recurrence of gliomas, significantly outperforming traditional methods that typically only achieve about 50% accuracy.
What challenges do pediatric patients face regarding cancer recurrence monitoring?
Pediatric patients often face significant challenges during cancer recurrence monitoring, including the stress and burden of frequent MRI scans. Traditional follow-up methods can become overwhelmingly demanding for children and their families, highlighting the need for advanced predictive tools utilizing AI to streamline the monitoring process.
Can machine learning improve pediatric glioma research outcomes?
Yes, machine learning can greatly enhance pediatric glioma research outcomes by providing more precise predictions of cancer recurrence. By utilizing advanced algorithms and temporal learning, researchers can analyze longitudinal data from multiple scans, improving the understanding of tumor behavior and helping to tailor treatment approaches more effectively.
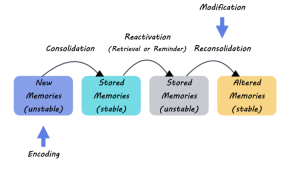
What role does temporal learning play in predicting pediatric cancer recurrence?
Temporal learning enhances prediction capabilities by training AI models on sequences of brain scans taken over time, allowing the model to detect subtle fluctuations that indicate potential recurrence of pediatric cancers like gliomas. This innovative approach significantly improves the model’s accuracy compared to traditional methods focusing on single images.
How might AI change the future of monitoring pediatric cancer recurrence?
AI holds the potential to transform the future of monitoring pediatric cancer recurrence by providing accurate risk assessments, which could lead to a reduction in unnecessary imaging for low-risk patients and the implementation of early interventions for high-risk patients. This shift could significantly improve patient care and quality of life.
| Key Point | Details |
|---|---|
| AI Tool’s Accuracy | The AI tool can predict relapse risk in pediatric glioma patients with 75-89% accuracy, outperforming traditional methods with 50% accuracy. |
| Temporal Learning Technique | This method uses multiple brain scans over time to train the AI, improving its predictive capabilities. |
| Clinical Implications | The researchers aim to conduct clinical trials to see if AI can enhance patient care by optimizing follow-up frequency and treatments. |
| Study Funding | Funded by the National Institutes of Health, leveraging partnerships with notable hospitals to gather nearly 4,000 MR scans. |
Summary
Pediatric cancer recurrence poses significant challenges for patients and families alike. Recent advancements have shown that AI tools can dramatically enhance predictions of relapse risk in children suffering from gliomas. By analyzing multiple brain scans over time, researchers can accurately identify those at the highest risk, potentially reshaping the standards of care. This innovative approach not only seeks to lessen the emotional and physical stress from frequent imaging but also aims to tailor treatments to individual needs based on the identified risk levels.